Welcome to question of the day #13
What is the van Herick technique?
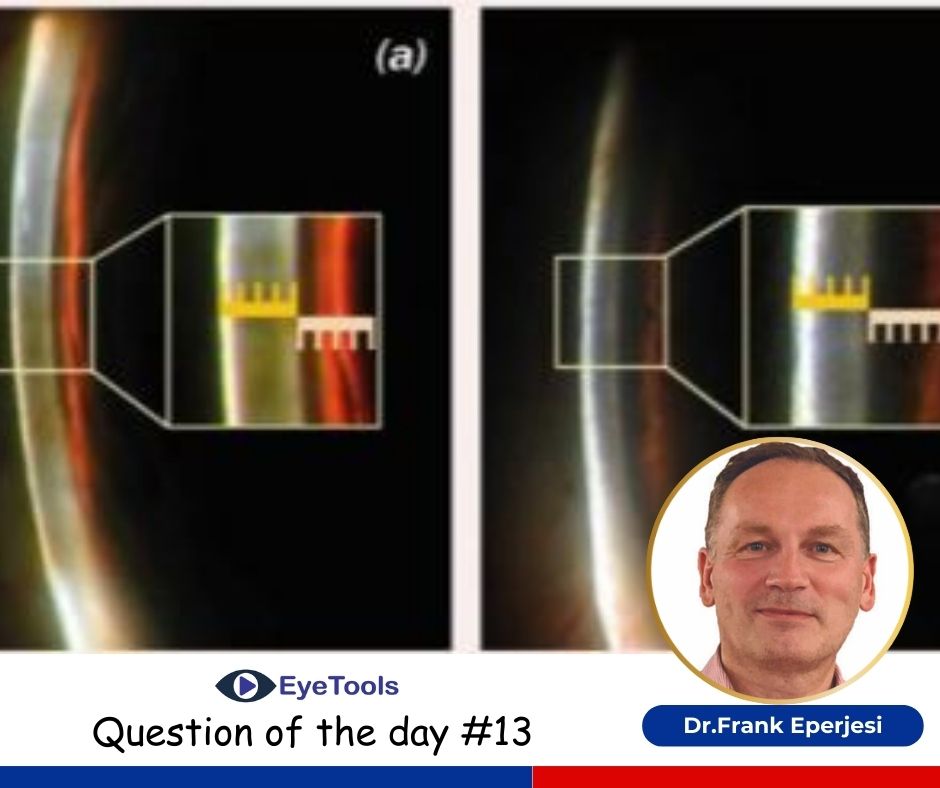
The depth of the anterior chamber angle can be estimated by the van Herick technique. This is performed using a sharply focused optic section positioned on the cornea at the very edge of the limbus. The cornea will be seen in cross-section with the slit beam reflected off the front surface of the iris. In the presence of an open anterior chamber angle and clear aqueous humour, the anterior chamber is optically empty and appears as a black space between the cornea and iris. The width of the space formed by the anterior chamber angle relative to the width of the corneal section is used as a measure for the angle width estimation.
Use
This technique may elicit the first clinical sign of narrow-angle or acute angle closure glaucoma in the symptomatic patient who presents acutely. Angles that are identified as being very narrow with this technique should be further evaluated with a goniolens. Frequently angles will be shown to be larger with this procedure than the van Herrick technique suggested. The technique can be used in the differentialdiagnosis of red eye e.g. viral conjunctivitis and closed angle glaucoma, closed angle and open angle glaucoma and acute and chronic glaucoma.
Slit lamp set up
- Coupled
- 60 degrees beam angle
- Beam width equivalent to an optic section
- Maximum beam height
- No filter
- Medium illumination
- 10-16X magnification.
Procedure
Place a narrow slit as close to the limbus as possible and normal to the cornea.
Narrow the beam to an optic section and instruct the patient to look straight ahead.
Focus the beam sharply on the cornea at the very edge of the temporal limbus.
Compare the width of the ‘shadow’ formed on the iris (representing the depth of the anterior chamber) to the width of the optic section (representing the thickness of the cornea).
The shadow is a dark interval between the light on the cornea and the light on the iris, that represents the optically empty aqueous in the anterior chamber.
The procedure should be repeated for the nasal limbus. The angle can be graded as follows:
Grade 4-the ratio of aqueous to cornea is 1:1-open angle
Grade 3-the ratio of aqueous to cornea is 1:2
Grade 2-the ratio of aqueous to cornea is 1:4-indicates narrow angle, which could be viewed by gonioscopy.
Grade 1-the ratio is smaller than 1:4-indicates dangerously narrow angle, which is likely to close.
If the grades of the nasal and temporal angles are judged to be different, both readings should be recorded.
Hints and tips
Errors in angle estimation may occur if the patient’s eyes are not in primary gaze.
The most common mistake that will result in angle overestimation is if the optic section is not placed far enough peripherally at the corneo-scleral junction.
The beam should be at exactly 60 degrees to the observation system.
Most slit lamps will have a scale for judging this angle.
Novice practitioners often have too wide a beam; it should be just thick enough to avoid extinction.



1.jpg)



.jpg)
.jpg)



_(Instagram_Post).jpg)
.jpg)
_(1080_x_1080_px).jpg)


with_UP_Cabinet_Minister_Sh_Nand_Gopal_Gupta_at_OpticsFair_demonstrating_Refraction.jpg)
with_UP_Cabinet_Minister_Sh_Nand_Gopal_Gupta_at_OpticsFair_demonstrating_Refraction_(1).jpg)

.jpg)








.jpg)



.png)




